Let’s be honest: navigating healthcare can sometimes feel like you’re a cog in a giant, impersonal machine. Rushed appointments, confusing jargon, treatment plans that feel one-size-fits-none… it’s the opposite of feeling truly seen and heard.

We talk endlessly about “patient-centered care,” but making it a reality has been a stubborn challenge. Enter Artificial Intelligence.
- Beyond the Clipboard: AI as Your 24/7 Health Concierge (Who Actually Listens)
- Your Body's Unique Blueprint: How AI Crafts Truly Personalized Care Plans (Not Just Best Guesses)
- Freeing the Human Healer: Why Less Admin for Docs Means More You Time
- Closing the Gap: Can AI Be Healthcare's Unexpected Equity Champion?
- The Empathy Algorithm? How AI Understands What You Aren't Saying
- Conclusion: The Symphony of Care
Before you picture cold robots taking over, hold on. What if AI, used thoughtfully, could actually be the key to humanizing your healthcare experience?
What if it could free up your doctor to truly listen, tailor care uniquely to you, and ensure you never feel lost in the system? This isn’t about replacing the human touch; it’s about amplifying it.
Let’s explore how smart technology is quietly revolutionizing care to put you, the patient, firmly back in the center – where you belong.
Beyond the Clipboard: AI as Your 24/7 Health Concierge (Who Actually Listens)
Remember that sinking feeling? It’s 2 AM. Your kid spikes a fever, or that weird new symptom you noticed during the day suddenly feels really urgent. You’re stressed, maybe a little scared.
You call the clinic… only to get an automated message telling you the office opens at 8 AM. Or worse, you finally get through the next day, navigate the phone tree, wait on hold, explain your situation again to the front desk, only to be told the next available appointment is weeks away. It feels like shouting into a void.
This is where AI steps in, not as a cold automaton, but as your tireless, always-available health concierge. Think less “robotic operator,” more like that incredibly efficient, calm, and listening hotel concierge who magically knows what you need before you even ask.

AI-powered chatbots or virtual assistants aren’t just answering machines. They’re sophisticated listeners. They can triage your concerns instantly, 24/7. Describe your symptoms in your own words (“My head is pounding and I feel nauseous when I look at screens”), and the AI doesn’t just hear keywords; it understands context.
It can ask clarifying follow-up questions just like a human would (“Is the pain behind one eye? Any vision changes?”), guiding you to the right level of care – whether that’s immediate ER attention, a same-day telehealth visit, self-care instructions, or reassurance that it’s likely a migraine and here’s how to manage it.
No hold music required. (Wondering just how well AI understands? We dug into the nuances of AI accuracy in diagnosis).
Your Personal Health FAQ, Answered Instantly:
Got a question about medication side effects right now? Need clarification on pre-op instructions at 10 PM? Confused by your lab results that just popped up in the portal? Your AI concierge can pull from vast, verified medical databases and your own health history (with your permission, of course) to give you clear, personalized answers instantly. No more frantic Googling leading down WebMD rabbit holes. It cuts through the noise, giving you reliable info tailored to your situation.
Remembering the Details Humans (Understandably) Forget:
Ever feel like you have to re-tell your entire medical history every time you see a new specialist or even a different nurse? AI acts as a seamless continuity thread. It can securely track your symptoms over time, note your preferences (like “I prefer email over phone calls”), and remember past concerns.
This means when you do connect with a human provider – whether via telehealth or in person – they walk in already briefed. They know the backstory.
That precious face-to-face time isn’t wasted on administrative catch-up; it’s focused entirely on you, your concerns right now, and building that vital human connection. (This efficiency isn’t just good for you – it’s a major factor in how AI reduces overall healthcare costs for everyone).
Especially for the tough stuff(like Mental Health)
The 2 AM anxiety spike is real. Reaching out can feel daunting. AI concierges can be a crucial first point of contact, offering immediate resources, coping strategies, grounding exercises, or simply a non-judgmental space to articulate what you’re feeling.
They can help bridge the gap until you can connect with a human professional, making that first step feel less overwhelming. (This naturally raises big questions about AI’s role – explore the boundaries in our pieces on whether AI can diagnose mental illness and if it could ever replace mental health professionals).
The Point Isn’t Replacement, It’s Reclamation. This AI concierge doesn’t take away the human doctor or nurse; it protects their time and expertise for the complex, deeply personal interactions that truly matter. It handles the routine, the informational, the logistical – the stuff that often makes healthcare feel frustratingly impersonal – so the humans can focus on what humans do best: care, empathy, and nuanced judgment. Suddenly, that rushed 10-minute appointment has the potential to feel like a focused 10-minute conversation.
So, your concierge listens and guides. But how does that translate into care that feels like it was designed specifically for you, down to your unique biology? Let’s talk about moving beyond best guesses to your true personal blueprint…
Your Body’s Unique Blueprint: How AI Crafts Truly Personalized Care Plans (Not Just Best Guesses)
Think about the last time you got a treatment plan. Did it feel… standard? Like maybe it was designed for “people with condition X” in general, but not necessarily for you, with your specific quirks, history, lifestyle, and even genetics?
That “one-size-fits-none” approach isn’t just frustrating; it can be downright ineffective, or even risky. We’ve all heard the stats: a drug that works wonders for one person might do nothing for another, or cause nasty side effects in someone else. This is where AI moves us light years beyond educated guesses. It’s not just plugging your symptoms into a flowchart. It’s about assembling a hyper-detailed, dynamic blueprint of you.
Decoding the Data Deluge (That Humans Can’t Handle):
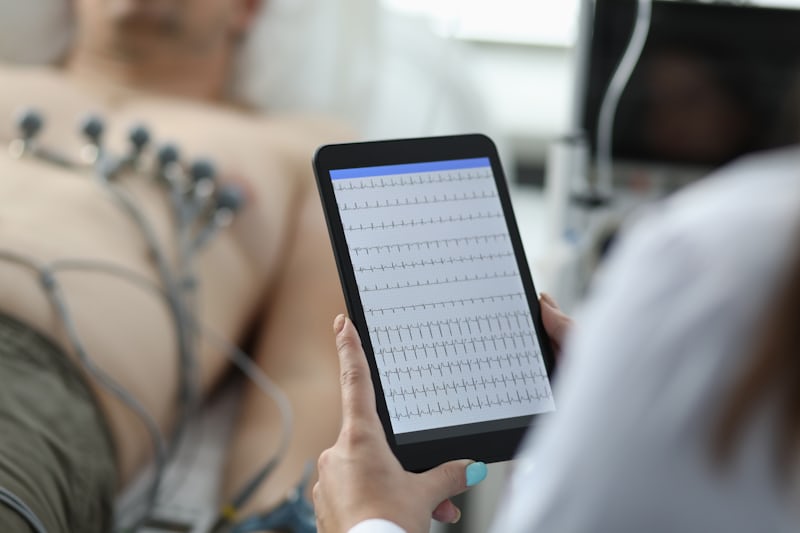
Your health story is written in mountains of data: years of lab results, imaging scans, doctor’s notes (often buried in dense text), wearable sensor readings (heart rate, sleep, activity), genetic markers, even your reported symptoms and lifestyle factors.
A human clinician, no matter how brilliant, simply can’t process and cross-reference all of this in real-time for every patient. AI can. It sifts through this avalanche, spotting subtle patterns, correlations, and risk factors that would be invisible to the naked eye. It’s like having a super-powered detective dedicated solely to understanding your biological narrative. (Curious about how AI interprets the complex ‘language’ within some of this data, like proteins? Our piece on [Protein Language Models])

Predicting Your Path, Not the Average One:
Forget generic population statistics. AI can build predictive models tuned to your blueprint. Based on your unique data mix, it can help forecast things like:
- “You have a 75% higher likelihood than average of developing side effect Y with medication Z – let’s consider alternative A.”
- “Given your specific genetic markers and current lifestyle, your risk of developing condition B in the next 5 years is elevated by X% – here’s a personalized prevention plan that actually fits your life.”
- “Your recovery trajectory from this procedure typically looks like this based on similar patients with your exact physiology – let’s tailor your rehab accordingly.”
This shifts medicine from reactive (“Let’s treat this problem now”) to proactive (“Let’s prevent your likely problems”).
Dynamic, Living Plans, Not Static Paperwork
Your life changes. Your health changes. A static care plan printed at one appointment is often obsolete by the next. AI enables dynamic personalization.
Imagine a plan that: Adjusts medication suggestions based on new lab results instantly flagged by the AI. Modifies exercise recommendations because your wearable data shows you’re consistently falling short (or exceeding!) the original targets.
Sends a gentle nudge about nutrition when your glucose trends suggest a pattern. Alerts your care team before a minor symptom you logged in an app becomes a major issue. It’s care that evolves with you, in real-time.
Beyond Disease: Personalizing Prevention & Wellness
This isn’t just for the sick. AI can analyze your unique blueprint to craft hyper-personalized wellness strategies. What’s the optimal sleep duration for you based on your activity and stress markers?
What specific nutrients might your body be craving based on genetic predispositions and diet logs? What type of exercise yields the best results for your metabolism? It turns generic health advice into bespoke wellness roadmap.
It’s the difference between being handed an off-the-rack suit and having one meticulously tailored to your exact measurements. One might fit okay. The other fits perfectly because it was designed exclusively for you
. AI is the master tailor, using the intricate measurements of your unique biology and life to craft care that finally feels like it truly fits.
Okay, so AI is crunching your data and designing your perfect plan. But what about the humans? Does this push doctors aside? Quite the opposite. Let’s see how AI is actually freeing them up to be more human than ever…

Freeing the Human Healer: Why Less Admin for Docs Means More You Time
Let’s play a quick game. Imagine your doctor’s 15-minute appointment. Now, guess how much of that precious time they actually spend looking at you.
If you guessed less than half… you’re sadly close. Studies show doctors spend up to 49% of their face-to-face clinic time staring at a computer screen. Clicking boxes. Typing notes. Wrestling with clunky electronic health records (EHRs).
It’s called “pajama time” for a reason – because so much of that documentation spills over into their nights and weekends. This isn’t just annoying; it’s soul-crushing burnout fuel and creates a massive empathy deficit. You feel rushed. They feel like data clerks.
This is where AI becomes the ultimate admin sidekick. It’s not about replacing the doctor; it’s about unshackling them. Think of it as taking the mountain of paperwork off their shoulders so they can finally sit down, breathe, and be your doctor.
The Invisible Scribe
Imagine an AI that actively listens to your natural conversation with your doctor. Using advanced speech recognition and Natural Language Processing (NLP), it can draft accurate clinical notes in real-time, highlighting key concerns, decisions, and follow-ups.
No frantic typing, no fragmented eye contact. Just a smooth, focused dialogue. The doctor reviews and finalizes it later in a fraction of the time. (Wondering how well AI understands complex medical conversations? Our deep dive on AI accuracy in diagnosis, touches on the core tech that makes this possible).

Pre-Visit Prep & Post-Visit Follow-Up, Automated
AI can analyze your records before you even walk in, flagging relevant trends or gaps to the doctor. Need a referral or prescription refill? AI can handle the initial requests and paperwork, routing only exceptions to the human.
After your visit, it can automatically generate personalized summaries for you and send reminders for tests or follow-ups. It’s like having an ultra-efficient coordinator working silently in the background.
Prior Auths? Let AI Fight That Battle
The time-sucking nightmare of insurance prior authorizations? AI systems can gather necessary clinical data, populate forms, submit requests, and even track their status – significantly reducing delays and staff frustration.
This is a major pain point contributing to burnout, and AI tackles it head-on. (This relentless admin grind is a key driver of inefficiency – see how tackling it contributes to broader healthcare cost reduction).
From Screen Gaze to Human Gaze
The real magic happens when you reclaim those minutes. Instead of your doctor’s fingers flying over a keyboard, they might:
- Actually listen without distraction.
- Notice the subtle worry in your eyes you didn’t mention.
- Explain that complex diagnosis with patience, using drawings or models.
- Ask, “How is this really affecting your life?” and have time to hear the answer.
- Collaborate with you on decisions, feeling less rushed.
The Ripple Effect: Less burned-out doctors stay in practice longer.
More present doctors make fewer errors. And you?

You get the undivided attention and deep expertise you came for. That feeling of being truly heard?
That’s patient-centered care in action, powered by AI taking the administrative drudgery off the humans’ plates. It’s not just efficiency; it’s restoring the heart of the healer-patient relationship.
Closing the Gap: Can AI Be Healthcare’s Unexpected Equity Champion?
Let’s face an uncomfortable truth: your zip code, your income, the color of your skin – they shouldn’t dictate the quality of your healthcare. But tragically, they often do.

Specialist deserts in rural areas. Long waits in underserved urban clinics. Implicit bias affecting diagnosis and treatment. Language barriers. The cost of taking time off work. These inequities are systemic and stubborn.
Could AI, often criticized for potentially amplifying bias, actually be part of the solution? Used intentionally and ethically, yes, absolutely. It’s emerging as a surprisingly powerful tool for leveling the playing field.
Bridging the Geographic Divide (Telehealth’s AI Copilot)
Virtual visits are great, but what if you live hours from a specialist? AI supercharges telehealth. Imagine a patient in a rural clinic with a complex skin lesion. A primary care provider uses a smartphone app with AI-powered image analysis. The AI provides immediate differential diagnoses and confidence levels, guiding the PCP during the telehealth consult with the distant dermatologist.
The specialist gets a pre-analyzed case, making their remote assessment faster and more accurate. This isn’t science fiction; it’s happening. AI acts as a force multiplier for scarce specialist expertise, bringing it virtually anywhere. (This democratization of expertise is a core theme in building the future of better healthcare)
Tearing Down Language Barriers in Real-Time
Medical jargon is hard enough in your native tongue. AI-powered translation tools integrated into patient portals, chatbots, and telehealth platforms can provide near real-time, accurate translation during conversations and for educational materials.

This empowers non-native speakers to understand their care, ask questions confidently, and feel respected – not just managed.
Bias Detection & Mitigation (The Guardrail Role)
Humans have bias – unconscious or otherwise. AI, trained on diverse datasets and designed with fairness as a core principle, can act as a crucial checkpoint. It can flag potential disparities in care recommendations (e.g., suggesting less pain medication for certain demographics without clinical reason) or identify patterns suggesting systemic bias within an institution’s own practices.
It prompts clinicians and administrators to pause and ask, “Is this truly equitable?” (This is complex, especially in sensitive areas like mental health – understanding the limits is key, as discussed in Can AI Diagnose Mental Illness?).
24/7 Access to Triage & Basic Care (Lowering the Barrier to Entry)
For communities facing long wait times or lacking transportation, that AI “health concierge” we talked about earlier is revolutionary. Getting immediate, non-judgmental triage, basic information, and guidance on whether and where to seek care (urgent care vs. ER vs. self-care) at 1:24 AM from your phone removes a huge initial barrier. It empowers individuals to navigate the system more effectively from the start.

Data-Driven Insights to Target Resources
AI can analyze population health data to pinpoint exactly where disparities are most acute – specific neighborhoods, specific conditions, specific demographic groups. This allows health systems and policymakers to direct resources (mobile clinics, community health workers, targeted screening programs) far more effectively than guesswork ever could.
The Crucial Caveat
AI isn’t a magic equity wand. It can perpetuate or worsen bias if trained on flawed, non-representative data or designed without equity as a core goal. Vigilance, diverse development teams, and constant auditing are non-negotiable.
But when built and deployed responsibly, AI offers tools to dismantle barriers we’ve struggled with for decades. It’s not about replacing the hard work of systemic change; it’s about providing powerful new instruments to help do that work faster and smarter. That’s a champion we desperately need.
The Empathy Algorithm? How AI Understands What You Aren’t Saying
We’ve all been there. Sitting in the exam room, putting on a brave face. “I’m fine, really,” you say, while inside, you’re swirling with worry, confusion, or even despair. Maybe you downplay your pain because you don’t want to seem “difficult.” Maybe you’re too overwhelmed to articulate the sheer impact that fatigue is having on your life. Or perhaps cultural norms make expressing certain fears feel taboo.
Here’s the uncomfortable truth: Humans miss things. Busy clinicians, even the most compassionate ones, can overlook subtle cues buried under layers of stoicism, language barriers, or sheer clinical complexity.
What if AI could help hear the whispers we don’t – or can’t – voice aloud? Don’t mistake this for artificial empathy. AI doesn’t feel your pain. But it’s becoming astonishingly adept at detecting the signals of human struggle hidden in plain sight.

Reading Between the Lines (of Your Words)
Advanced Natural Language Processing (NLP) goes far beyond keyword spotting. When you type a message into a patient portal describing your symptoms, or when an AI analyzes transcripts of telehealth calls (with consent!), it can detect:
- Sentiment Shifts: A gradual increase in words denoting frustration, helplessness, or fear over time.
- Hedging & Minimization: Phrases like “It’s probably nothing,” “It’s just a little ache,” or “I guess I’m managing,” which often mask significant distress.
- Inconsistencies: Discrepancies between what you report (“Sleeping okay”) and data from wearables (showing severely disrupted sleep patterns).
- Unmet Needs: Reading frustration in repeated questions about side effects that haven’t been adequately addressed.
This isn’t mind-reading; it’s pattern recognition at superhuman scale, flagging potential emotional or social distress a human might miss in the clinical rush.
The Tone Beneath the Words
Beyond what is said, AI can analyze how it’s said during audio interactions (again, ethically and with permission):
- Vocal Biomarkers: Subtle changes in speech pace, pitch, pauses, or even vocal cord tension can indicate anxiety, depression, or pain levels that a patient isn’t verbally reporting.
- Facial Expression Analysis (Ethically Applied): In video visits, AI can (controversially, and requiring strict ethical frameworks) identify fleeting micro-expressions indicative of pain, confusion, or fear that flash across a face faster than a human eye can register.
The key is using this not for diagnosis, but as a gentle prompt to the clinician: “Hey, the patient just described their pain as ‘manageable,’ but their vocal stress spiked significantly. Maybe probe a bit deeper?”
Connecting the Dots Across Data Silos
Your social determinants of health matter. AI can correlate clinical data with broader context (anonymized and aggregated ethically): A sudden drop in medication adherence flagged by a pharmacy feed, coinciding with a change of address to a known transit desert. Frequent ER visits for non-specific complaints aligning with social media posts (if publicly available and ethically sourced) suggesting job loss or housing instability. This paints a picture not just of disease, but of life circumstances impacting health, prompting the care team to ask, “What support do you really need right now?”

Especially Critical in Mental Health: These signals are vital for conditions where self-reporting is incredibly difficult. Flagging subtle linguistic markers of suicidal ideation, detecting vocal flatness associated with severe depression, or noticing a withdrawal from digital interactions can be crucial prompts for timely, compassionate human intervention. (This highlights why AI is a tool within mental health, not a replacement, as we discussed in Can AI Replace Mental Health Professionals?).
The Crucial Human Handoff
This is where the magic truly happens. AI acts like a highly sensitive radar, picking up faint distress signals. It doesn’t interpret them definitively, and it never responds alone. It alerts the human care team: “There might be more going on here emotionally or socially. Please check in.”
This empowers nurses, doctors, therapists, and social workers to approach the conversation with deeper insight and focused empathy: “I noticed you mentioned feeling ‘okay,’ but your tone sounded a bit strained when talking about work. How are things *really* balancing?”
The Result?
Patients feel seen on a level that often surprises them. Care becomes less about just treating the charted symptom and more about addressing the whole, complex human being behind it. It transforms “What’s the matter?” into “What matters to you?” – and that’s the beating heart of patient-centered care.
Conclusion: The Symphony of Care
So, where does this leave us? Not with a cold, robotic takeover, but with a powerful, nuanced.
AI isn’t the soloist; it’s the section providing the underlying structure, the intricate counter-melodies, freeing up the human musicians – your doctors, nurses, therapists – to perform their most profound work: the melody of connection, empathy, and judgment that only humans can create.

From your tireless 24/7 health concierge ensuring you’re never lost in the void, to the master tailor crafting care plans from your unique biological blueprint; from liberating healers from soul-crushing paperwork so they can truly see you, to fighting inequity and amplifying unheard voices; and finally, to sensing the unspoken struggles whispering beneath the surface – AI, when designed and deployed with intention and ethics, is proving to be an indispensable instrument in creating healthcare that finally, genuinely, revolves around you.
It’s not about technology for technology’s sake. It’s about harnessing these tools to reclaim the time, the attention, the personalization, the access, and the deep understanding that transforms care from a transaction back into a human relationship.
That’s the future of patient-centered care – and it’s being written now.
